Yellow fever
Yellow fever is caused by a virus, which circulates between infected monkeys or humans and mosquitoes
Key messages
-
Yellow fever (YF) is a viral disease transmitted by mosquitoes causing a spectrum of disease from mild to severe symptoms.
-
Mosquito bite avoidance and yellow fever vaccination is recommended for travellers visiting countries where there is a risk of YF virus transmission.
-
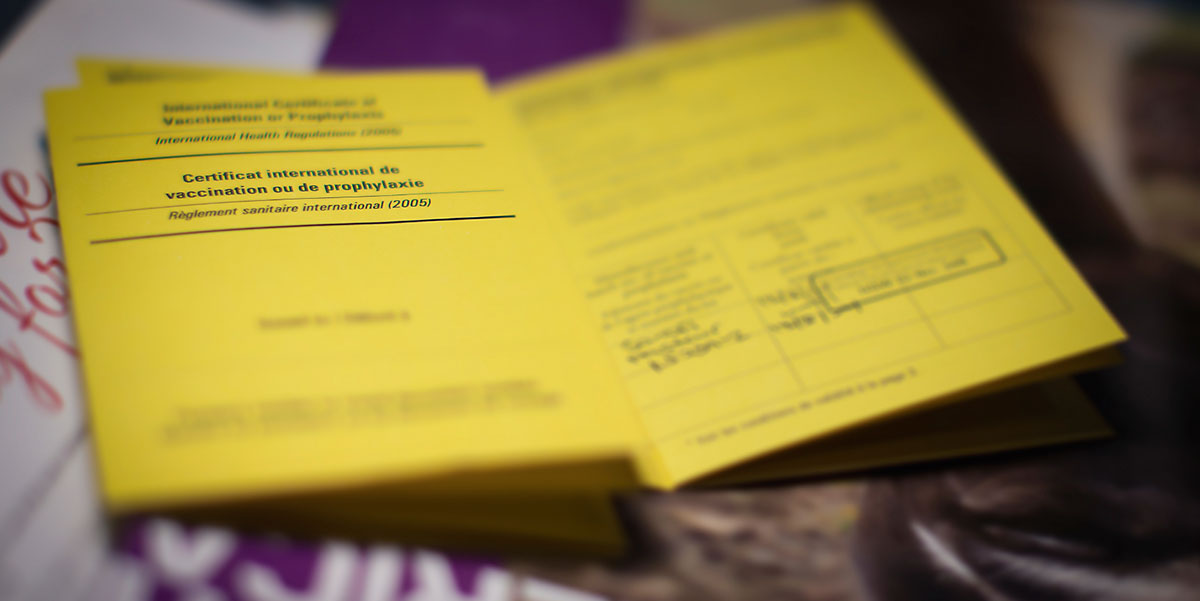
Under the International Health Regulations (2005), an International Certificate of Vaccination or Prophylaxis for YF may be an entry requirement for some travellers to YF risk countries.
-
YF certificate requirements are not necessarily connected to the risk of disease for a traveller.
-
The YF vaccine is only available at designated UK Yellow Fever Vaccination Centres (YFVCs).
-
There is no treatment for YF disease. Care of an infected person is based on managing the symptoms.
Overview
Yellow fever (YF) is caused by a virus of the Flaviviridae family, which circulates between infected monkeys or humans, and mosquitoes.
YF virus can cause an illness that results in jaundice (yellowing of the skin and eyes) and bleeding with severe damage to the major organs (e.g. liver, kidneys and heart). The mortality rate is high in those who develop severe disease.
YF is a vaccine preventable disease. In order to prevent the international spread of YF, under the International Health Regulations (IHR) (2005) [1], countries may require proof of vaccination, recorded in an International Certificate of Vaccination or Prophylaxis (ICVP). A Medical Letter of Exemption (MLoE) from vaccination, which should be taken into consideration by a receiving country, can be provided where a health professional advises that an individual should not be vaccinated on medical grounds.
Risk areas
There is a risk of YF transmission in parts of the tropical and sub-tropical regions of Africa and South and Central America and in Trinidad (Caribbean).
Areas with a 'risk of YF transmission' (also known as endemic areas) are countries (or areas within countries) where mosquito species known to transmit the disease are present and where the infection is reported in monkeys and/or humans.
Some areas are designated as having a low potential for exposure to yellow fever; these are bordering endemic areas where there have been no confirmed reports of yellow fever in either monkeys or humans, and evidence of transmission in the past is uncertain or suggests low prevalence of infection. Transmission of YF virus in these areas is therefore considered unlikely [2].
Under-reporting, limitations in surveillance methods and misdiagnosis make estimating the burden of YF disease challenging [3]. Historically, the World Health Organization (WHO) estimated 200,000 cases of YF and 30,000 deaths occurred globally each year, with the majority (90 percent) occurring in Africa. These estimates were based on studies from the early 1990s. A study of YF disease burden in Africa in 2013 estimated there to be 130,000 (51,000–380,000) cases of severe YF, resulting in 78,000 (19,000–180,000) deaths [3]. However, more recent modelling data estimate 100,000 (63,000–158,000) cases of YF occur in Africa annually, with 47,000 (29,000–75,000) deaths. In South America, estimates suggest 8,000 (4,000–15,000) cases, with 4,000 (2,000–7,000) deaths annually [4].
Following a consultation on YF and international travel, convened by the WHO in 2008, an expert working group considered the evidence for risk of YF transmission on a country-by-country basis [2, 6].
Table 1: Countries with a risk of yellow fever transmission as defined by the World Health Organization
See current Countries with risk of yellow fever transmission and countries requiring yellow fever vaccination 'Annex 1' and Vaccination requirements and recommendations for international travellers 'country list' on WHO Travel advice page
| Africa | Central and South America |
| Angola Benin Burkina Faso Burundi Cameroon Central African Republic Chad* Congo Côte d'Ivoire (Ivory Coast) Democratic Republic of the Congo Equatorial Guinea Ethiopia* Gabon The Gambia Ghana Guinea Guinea-Bissau Kenya* Liberia Mali* Mauritania* Niger* Nigeria Senegal Sierra Leone South Sudan Sudan* Togo Uganda |
Argentina* Bolivia* Brazil* Colombia* Ecuador* French Guiana Guyana Panama* Paraguay* Peru* Suriname Trinidad and Tobago* Venezuela* |
*Only some parts of this country have a risk of yellow fever disease. Remaining areas either have low potential for yellow fever transmission or no risk.
Table 2: Countries with low potential for exposure to yellow fever as defined by the World Health Organization
| Africa |
| Eritrea* Rwanda** Sao Tome and Principe** Somalia* Tanzania** Zambia* |
*Low potential for exposure to yellow fever in some parts of this country
**Low potential for exposure to yellow fever throughout this country
Areas at risk of transmission are dynamic and subject to change. There may be lengthy periods between outbreaks of YF, nevertheless, in endemic areas, the virus may still be circulating, but at a level that is not identified through surveillance. Please watch this website for updates and refer to our Country Information pages for individual country recommendations and vaccine recommendation maps.
Risk for travellers
The risk of contracting YF is determined by the following factors:
- travel destination
- intensity of YF transmission in area to be visited
- season of travel (most cases in travellers have occurred in the late rainy season to early dry season)
- duration of travel
- activities allowing exposure to mosquitoes
- immunisation status [7]
Although ongoing cases and outbreaks of YF occur in Africa and South America, the disease is preventable by vaccination and remains a very rare cause of illness in travellers.
In December 2015, an outbreak of YF was reported in Angola. The World Health Organization described this as Angola's worst YF outbreak in 30 years [8]. Imported cases in travellers returning from Angola were reported from China, Democratic Republic of the Congo and Kenya [8-10].
Between August 2016 and 14 March 2017 the European Centre for Disease Prevention and Control (ECDC) reported that four cases of YF had been reported in European travellers who visited YF risk regions in South America [11]. Two YF cases, one fatal, were reported in French travellers to Peru on 10 August 2016. A third case, in a Danish traveller to Bolivia, was confirmed on 13 February 2017 [12]. The fourth case, in a Dutch traveller to Suriname, was reported on 13 March 2017 [13]. None of these four travellers had been vaccinated against YF [11].
In October 2016, an unvaccinated traveller from USA was diagnosed with yellow fever after returning from the Amazon area of Peru [14].
In January 2018, the WHO reported a case in an unvaccinated traveller from the Netherlands who had visited the State of Sao Paulo, Brazil [15]. Since this report, a number of other cases have been reported in unvaccinated travellers from Europe, Argentina and Chile who had visited Brazil [16].
Prior to these cases, between 1970 and 2015 a total of ten YF cases were reported in unvaccinated travellers from Europe and the United States who visited South America or West Africa [17].
In 1930, a laboratory worker in the UK contracted YF while working with the virus at the Hospital for Tropical Diseases in London [18].
Outbreak reports can be helpful when undertaking a risk assessment for travellers. However, it is important to acknowledge the limitations of such reports; case numbers and outbreaks may not accurately represent YF activity and reporting systems and the level of information that is sent to the WHO may differ between countries.
International Health Regulations (2005)
The International Health Regulations (IHR) were revised and adopted by the World Health Assembly in 2005. They were formulated to help prevent the international spread of disease, and in the context of international travel, do so with minimum disruption to trade and travel. Under Annex 7 of the IHR (2005), YF has been designated as an infection for which an International Certificate of Vaccination or Prophylaxis (ICVP) may be required for travellers as a condition of entry to a country. Other diseases may be designated if WHO put in place temporary recommendations as a result of an outbreak being declared a Public Health Emergency of International Concern (PHEIC). Currently YF and polio are the only diseases for which an ICVP may be required for entry into or exit from a country [1].
As of 11 July 2016, WHO states that the period of validity of the ICVP has changed from 10 years to the duration of the life of the person vaccinated. This applies to all ICVPs for YF vaccination, including certificates already issued, and new or duplicate certificates [19].
Countries where YF does not occur, but where the mosquito vector and often the non-human primate hosts are present, are vulnerable to importation of YF and subsequent onward transmission within the local population. For these countries, YF vaccination may be an entry requirement for all travellers arriving from countries where there is a risk of YF transmission (often including airport transit through a country with risk of YF transmission).
Countries with risk of YF transmission may or may not require proof of YF vaccination from travellers. The absence of a requirement for YF vaccination does not necessarily mean that there is no risk of YF in the country, and YF vaccination may still be recommended for the protection of the individual traveller.
Member states are asked to submit details of their YF certificate requirements to WHO every two years. Information is published by the WHO on their Travel advice page and details can be found on our Country Information pages. Please note that between WHO updates, countries may change their certificate requirements. NaTHNaC will update the Country Information pages on TravelHealthPro when country updates have been officially confirmed.
When YF vaccine is required under IHR (2005), failure to provide a valid ICVP to the port health authorities could result in a traveller being quarantined, put under surveillance, or denied entry [1].
WHO states that valid certificates of vaccination presented by arriving travellers cannot be rejected on the grounds that more than ten years have passed since the date vaccination became effective as stated on the certificate; boosters or revaccination cannot be required [19].
If YF vaccination is contraindicated for medical reasons (including infants under 6 months of age), a MLoE from vaccination can be issued by an authorised health worker (e.g. in the UK the YFVC Responsible Supervising Clinician (RSC), a nurse, dentist or pharmacist working at that centre, or a licensed health professional otherwise supervising the medical care of the traveller).
Transmission
Jungle primates (e.g. susceptible species of monkey) and humans are the hosts for the YF virus [20]. The virus is transmitted (spread) via the bite of infected Aedes spp. (Africa and Americas) or Haemogogus spp. and Sabethes spp. (Central and South America only) mosquitoes. Only females of these mosquito species transmit the virus.
Transmission of YF occurs in three cycles:
- Jungle: occurring in tropical rainforests of Africa and South America. The transmission cycle occurs between monkeys and jungle breeding mosquitoes. Humans can become infected when they live or work in areas where this cycle occurs.
- Savannah (Africa only): occurs in the moist savannah regions of Africa where humans live and work close to the monkey population. The transmission cycle occurs between monkeys and humans, with spread via Aedes spp.
- Urban: following infection during the jungle cycle, infected humans can introduce the virus to urban areas where there is a high population density. Virus transmission occurs between humans in areas where the domesticated mosquito vector, Aedes aegypti (i.e. those that breed around human habitation) is present.
Aedes spp. mosquitoes are adapted to living in an urban (domestic) environment and breed in water collections provided by humans (e.g. vases, tyres and other receptacles); this species is active during daylight hours, and bite from dawn to dusk.
Haemagogous spp. and Sabethes spp. mosquitoes live in the forest canopy in Central and South America. These mosquitoes feed on monkeys; it is unclear if these mosquitoes have a predictable, preferred feeding time [CDC personal communication]. They can descend to ground level when the forest has been disturbed (e.g. during logging or during cultivation), where they may bite humans [21].
Once infected with the virus, the mosquito remains infectious for life (two to three months). Generally, mosquito species are most active at times of high rainfall, both in the jungle and urban environments. YF virus can survive very dry conditions in mosquito eggs, which hatch once a water collection is replenished. This can result in YF outbreaks in urban and rural areas, even during the drier months.
Signs and symptoms
YF varies in severity. The infection has an incubation period (time from infected mosquito feeding to symptoms developing) of three to six days. Initial symptoms include myalgia (muscle pain), pyrexia (high temperature), headache, anorexia (lack of appetite), nausea, and vomiting. In many patients there will be improvement in symptoms and gradual recovery three to four days after the onset of symptoms.
Within 24 hours of an apparent recovery, 15 to 25 percent of patients progress to a more serious illness. This takes the form of an acute haemorrhagic fever, in which there may be bleeding from the mouth, eyes, ears, and stomach, pronounced jaundice (yellowing of the skin, from which the disease gets its name), and renal (kidney) damage. The patient develops shock and there is deterioration of major organ function; 20 to 50 percent of patients who develop this form of the disease do not survive [22]. Infection results in lifelong immunity in those who recover.
Diagnosis and treatment
The preliminary diagnosis of YF is based on the patient's clinical features, location and dates of travel, and activities [17].
If a clinician suspects YF in a returned traveller, an urgent referral to an infectious disease/tropical disease clinical team is required.
UK Health Security Agency (UKHSA) Rare and Imported Pathogens Laboratory is a specialist centre for health professionals providing advice and diagnosis of a wide range of unusual viral and bacterial infections including yellow fever.
Preventing yellow fever
There are several methods to prevent YF infection: mosquito control, bite avoidance, and vaccination.
A highly effective live, attenuated (weakened) YF vaccine has been available for more than 80 years [7]. Vaccination is recommended for persons at risk of yellow fever infection. The contraindications and precautions (see below) for this vaccine should be considered according to individual risk assessment. Persons aged 60 years or older should only be given the vaccine when there is significant and unavoidable risk of acquiring YF infection, such as travel to an area where there is current or periodic risk of YF transmission (see Aged 60 years and older below).
Persons who travel to YF risk countries, or areas within countries with risk of transmission, without the benefit of vaccination should be advised of the risk of contracting YF. Meticulous mosquito bite avoidance measures are advised for all travellers [23].
Vaccine information
Country recommendations for YF vaccination
The recommendations for YF vaccination should be reviewed on our Country Information pages. Vaccine recommendation maps should be used alongside the Country Information page recommendations.
Recommendations for the use of the vaccine
YF vaccine is indicated for individuals at risk of yellow fever, and to prevent the international spread of this disease. The following groups should be immunised if there are no contraindications to the vaccine [23]:
- laboratory workers handling infective material
- persons aged nine months or older travelling to or living in countries with a risk of yellow fever transmission (see vaccination recommendation maps on the Country Information pages)
- persons aged nine months or older who are travelling to or living in countries that require an International Certificate of Vaccination or Prophylaxis (ICVP) for entry
Note that a requirement for an ICVP is not always related to the risk of exposure to YF disease.
Due to contraindications and precautions to this vaccine (see below), a careful assessment that balances the risk of YF disease with the risk of YF vaccine serious adverse events, should be undertaken. Individual risk assessment must consider many factors including the age and health status of traveller and details of the travel itinerary. As part of the Commission on Human Medicines (CHM) review of serious and fatal reactions following YF vaccine, the use of a standardised checklist to support medical history taking in the YF risk assessment is required [24].
All travellers who are vaccinated should be given the manufacturer's patient information leaflet. Travellers who received the vaccine should be informed about the early signs and symptoms of YF vaccine side effects and need to urgently seek medical attention if serious side effects are suspected [25] (see Adverse Events section below).
Travellers with contraindications to vaccination who must travel to an area where there is a requirement for an ICVP should carry a MLoE and take scrupulous care with mosquito bite avoidance. There may also be circumstances where there is no contraindication to vaccination but where the risk of vaccine adverse event is considered, after careful risk assessment, to be greater than the risk of disease (especially* where a precaution to vaccination is identified); in this scenario, where paperwork for entry to a country is a requirement, a MLoE may be an option (NaTHNaC opinion). Specialist opinion/advice can be sought.
*but not exclusively
Availability
There is currently one licensed YF vaccine in the UK, Stamaril® (Sanofi). This contains an attenuated 17D strain of YF virus and protects against all strains of YF.
The Summary of Product Characteristics (SPC) for the vaccine should be consulted for specific information relating to the product.
| Vaccine | Schedule | Length of protection | Age range |
| Stamaril® | 1 dose | At least 35 years and may be lifelong (*see below) | Minimum age 9 months. Seek medical advice for infants 6–8 months who are travelling to high-risk area |
*Reinforcing immunisation (booster dose) should be offered to a small subset of travellers who may be at continued risk see UKHSA [23].
A single dose confers immunity in 95–100% of recipients [23].
Contraindications
YF vaccine should not be given to the following groups under any circumstances [23]:
- infants aged under six months
- persons with a confirmed anaphylactic reaction to a previous dose of YF vaccine
- persons with a confirmed anaphylactic reaction to any of the components of the vaccine (see below for egg allergy)
- persons with a history of thymus disorder* or removal of the thymus gland for any reason (thymectomy) including incidental thymectomy (e.g. during cardiac surgery)
- persons with primary or acquired immunodeficiency due to congenital condition or disease process including symptomatic HIV infection and asymptomatic HIV infection when accompanied by evidence of impaired immune function
- persons who are immunosuppressed as a result of treatment, including high dose systemic steroids, immunosuppressive biologic therapy, radiotherapy or cytotoxic drugs (see Chapter 6, Immunisation against infectious disease and Precautions section below)
- persons with a first-degree** family history of YEL-AVD or YEL-AND following vaccination that was not related to a known medical risk factor (in case of an unidentified genetic predisposition)
- individuals aged 60 years and older travelling to countries and areas designated by WHO as areas with low potential for exposure to yellow fever virus (see section on people aged 60 years and older)
*including myasthenia gravis and thymoma
**close blood relative - parents, full siblings, or children
Precautions
For those with a febrile illness (fever) or who are acutely unwell, YF vaccination should be postponed until full recovery.
Where travel to YF risk areas is unavoidable, YF vaccination may be considered for the following groups after careful individual risk assessment and specialist advice (where appropriate):
- breast feeding women
- infants aged six to eight months
- individuals aged 60 years and older (see Aged 60 years and older below)
- those taking low dose steroid or non-biological oral immune modulating drugs
- individuals living with HIV (with a CD4 count greater than 200 and a suppressed viral load)
- pregnant women [23]
Individual risk assessment should consider the risk of the disease at the destination versus the potential for adverse events following YF vaccination (which may be greater where certain underlying medical conditions exist). Specialist opinion/advice may be advisable.
Health professionals should access the further information available on precaution groups in the following resources:
Adverse events
The 17D strain virus YF vaccine has been in use for more than 80 years. It is estimated that 500 million doses of the vaccine have been administered worldwide [7]. Reactions to YF vaccine are usually mild and short lived. They include myalgia (muscle pain), headache, and low-grade fever, typically occurring during the first five to ten days post vaccination and affecting 10–30% of recipients.
Serious adverse events are rare and fall into three main categories: hypersensitivity reactions, vaccine-associated neurologic disease (YEL-AND) and vaccine-associated viscerotropic disease (YEL-AVD).
Hypersensitivity reactions
The vaccine is propagated in chick embryos. The SPC for Stamaril® (the only YF vaccine used in the UK) lists sorbitol and lactose as excipients.
The SPC also states that the tip caps of the prefilled syringes contain a natural rubber latex derivative, which may cause allergic reactions in latex sensitive individuals.
Anaphylaxis, because of sensitivity to either egg or other vaccine components, is estimated to occur at an incidence of 1.3 cases/100,000 doses distributed (US data) [26].
Note: egg allergy is very common in younger children, yet many will outgrow their allergy by the time they reach school age. Travellers with a history of immediate-type egg allergy should be carefully risk assessed. See chapter 35 of 'Immunisation against infectious disease' for further guidance.
Yellow Fever Vaccine-Associated Neurologic Disease (YEL-AND)
Post-vaccine encephalitis has been recognised as a rare event since the early use of the vaccine. Cases were reported in very young infants during the 1950s (when there was no age restriction for vaccine administration). In the 1960s, when vaccine use was restricted to babies aged over six months, reduced numbers of post vaccine encephalitis were reported [7].
Since 2001, a new pattern of neurologic adverse events (undesirable effects on the nervous system) has been recognised [27-30]. These events have been termed YF vaccine-associated neurologic disease (YEL-AND); Reporting rates are estimated to be 0.8 cases per 100,000 doses distributed (US data); rates increased with increasing age (see below) [26].
The clinical presentation of neurologic events begins two to 56 days following receipt of vaccine (US data) [17], with fever and headache that can progress to encephalitis (inflammation of the brain), or an autoimmune demyelinating disease (a disorder that can interrupt nerve transmission) with peripheral or central nervous involvement. Most patients will completely recover. Almost all cases have occurred in those receiving the vaccine for the first time with no underlying YF immunity [17].
Yellow Fever Vaccine-Associated Viscerotropic Disease (YEL-AVD)
YF vaccine-associated viscerotropic disease (YEL-AVD) is a syndrome of fever and multi-organ failure that resembles severe YF disease; it was first described in 2001 [30]; over 100 confirmed and suspected cases have been reported worldwide [17]. Five cases have been reported in the United Kingdom, one in 1998, two in 2000 [31], and two fatal cases in 2018 and 2019 respectively [32].
One to eighteen days (median four days) following vaccination [17], patients with YEL-AVD develop fever, malaise, headache, and myalgia that progress to hepatitis (inflammation of the liver), hypotension (low blood pressure), and multi-organ failure. Death has occurred in more than 60 percent of reported cases worldwide [7]. In the US, the case-fatality ratio for all reported YEL-AVD cases is approximately 48 percent [17].
All reported cases of YEL-AVD have occurred in first-time vaccine recipients [7, 17].
YEL-AVD has been estimated to be reported in 0.3 cases per 100,000 doses distributed (US data). The rates increased with increasing age (see below) [26].
Aged 60 years and older
For individuals who are aged 60 years and older, the risk for these serious adverse events increases several fold to approximately 2.2 cases per 100,000 doses distributed for YEL-AND. For YEL-AVD the risk for those who are 60 years and older is 1.2 cases per 100,000 doses distributed and higher for those who are 70 years and older (US data) [26].
In people aged 60 years or older, due to a higher risk of life-threatening side effects, the vaccine should be given only when there is a significant and unavoidable risk of acquiring yellow fever infection, such as travel to an area where there is a current or periodic risk of yellow fever transmission [25].
Older travellers visiting areas with low potential for exposure to yellow fever virus
People aged 60 years or older should not be given the vaccine for areas designated by WHO as 'low potential for exposure to yellow fever' (i.e., areas where YF vaccination is 'generally not recommended', see table 2); such areas should be considered as not representing a 'significant and unavoidable risk' [23-25].
Thymus disorder or removal of thymus gland for any reason
Additional risk factors for serious adverse events following YF vaccination are thymus disorder and removal of the thymus gland (thymectomy) [33] for any reason [25]; and YF vaccine should never be given to individuals with this medical history [23-25].
Some cardiac surgical procedures may involve incidental thymectomy. Chapter 35 of 'Immunisation against infectious disease' provides guidance for both children and adults who have had cardiac surgery.
Family history of YEL-AVD or YEL-AND
There is currently insufficient evidence to determine if specific genetic risk factors pose an increased risk of serious adverse reactions; more research is needed in this area [24]. Until further information is available, YF vaccine should not be given to those who have a first-degree family history (i.e., blood relatives; parent, full sibling or child) of YEL-AVD or YEL-AND that was not related to a known medical risk factor (i.e., in case of an unidentified genetic predisposition) [25].
Further information on adverse events following YF vaccine is available in Immunisation against infectious disease, Chapter Ch. 35. Yellow fever.
YF and MMR/MMRV vaccine timing
A four-week minimum interval period should be observed between the administration of these vaccines. Yellow fever and measles, mumps and rubella vaccines (MMR) or measles, mumps, rubella and varicella vaccine (MMRV)should not be administered on the same day. Co-administration of these vaccines can lead to sub-optimal antibody responses to YF, mumps and rubella antigens. Where protection is required rapidly then the vaccines should be given at any interval; an additional dose of MMR/MMRV should be considered [34]. Re-vaccination with YF vaccine can be considered on a case-by-case basis for those at ongoing risk [23].
Resources
- World Health Organization: International health regulations (2005)
- World Health Organization: Yellow fever
- NaTHNaC: Yellow Fever Zone
- ICVP (YF or polio) and Hajj/Umrah certificate email enquiry service
- Yellow fever: information for travellers leaflet
References
-
World Health Organization. International Health Regulations (2005). Geneva: World Health Organization, 2005:1-60. [Accessed 7 May 2025]
-
World Health Organization. Yellow fever risk mapping: Background for the Consultation on Yellow Fever and International Travel, 2010. [Accessed 7 May 2025]
-
Garske T, Van Kerkhove MD, Yactayo S, Ronveaux O, Lewis RF, et al. (2014) Yellow Fever in Africa: Estimating the Burden of Disease and Impact of Mass Vaccination from Outbreak and Serological Data. PLoS Med 11(5): e1001638. doi:10.1371/journal.pmed.1001638 [Accessed 12 September 2022]
-
Gaythorpe KAM, Hamlet A, Jean K et al. The global burden of yellow fever. eLife. March 2021; 16, 10:e64670 [Accessed 7 May 2025]
-
World Health Organization. Wkly Epidem Rec. Vaccines and vaccination against yellow fever: World Health Organization Position Paper, June 2013; 27, 88:269-284. [Accessed 7 May 2025]
-
Jentes ES, Poumerol G, Gershman MD et al. The revised global yellow fever risk map and recommendations for vaccination, 2010: consensus of the Informal WHO Working Group on Geographic Risk for Yellow Fever. Lancet Infect Dis 2011; 11(8):622-632.
-
Staples JE, Monath TP, Gershman MD, Barrett ADT. Yellow fever vaccine Ch.63 In. Plotkin S, Orenstein W, Offit P, Edwards KM (Eds). Plotkin's Vaccines 7th ed. Philadelphia, 2017.
-
World Health Organization. Angola grapples with worst yellow fever outbreak in 30 years. 29 March 2016 [Accessed 7 May 2025]
-
World Health Organization. China. 22 April 2016. [Accessed 7 May 2025]
-
World Health Organization. Yellow fever - Kenya. Disease outbreak news, 6 April 2016 [Accessed 7 May 2025]
-
European Centre for Disease Prevention and Control. RAPID RISK ASSESSMENT Yellow fever among travellers returning from South America. 14 March 2017. [Accessed 7 May 2025]
-
Pan American Health Organization. Epidemiological Update Yellow Fever. 16 February 2017 [Accessed 7 May 2025]
-
Government of the Netherlands. Ministry of Health, Welfare and Sport. Patient with yellow fever. 13 March 2017. [Accessed 7 May 2025]
-
Newman A.P., Becraft, R. Dean A.B. et al Notes from the Field: Fatal Yellow Fever in a Traveler Returning from Peru - New York, 2016. MMWR September 1, 2017 / 66(34);914-915 [Accessed 7 May 2025]
-
World Health Organization, Yellow fever- Brazil. Disease outbreak news, 22 January 2018 [Accessed 7 May 2025]
-
Gossner CM,Haussig JM, de Bellegarde de Saint Lary C et al. Increases risk of Yellow fever infections among unvaccinated European travellers due to ongoing outbreak in Brazil. July 2017 to March 2018. Eurosurveillance. Vol 23, Issue 11, 15 Mar 2018 [Accessed 7 May 2025]
-
US Centers for Disease Control and Prevention. Yellow Fever. In: Health Information for International Travel. 2024 [Accessed 7 May 2025]
-
Cook GC. Fatal yellow fever contracted at the Hospital for Tropical Diseases, London, UK, in 1930. Trans Roy Soc Trop Med Hyg 1994; 88 (6): 712-3.
-
World Health Organization. Amendment to International Health Regulations (2005). Annex 7 (yellow fever). [Accessed 7 May 2025]
-
Young PR, Ng LFP, Hal RA et al. Arbovirus Infection Ch14. In: Farrar J, Hotez PK, Junhannss T et al (eds). Manson's Tropical Diseases. 23rd Edn. Elsevier (Saunders). 2014.
-
Service M. Medical Entomology for Students. 5th ed. New York. Cambridge University Press; 2012
-
Monath T, Cetron M. Prevention of yellow fever in persons travelling to the tropics. Clin Infect Dis. 2002; 24:1369-1378.
-
UK Health Security Agency. Yellow fever. Ch 35. In: Immunisation against infectious disease. 6 February 2024 [Accessed 7 May 2025]
-
Commission on Human Medicines. Yellow fever vaccine - report of the Commission on Human Medicine's Expert Working Group on benefit-risk and risk minimisation measures. November 2019. [Accessed 7 May 2025]
-
MHRA, PHE, NaTHNaC, HPS Yellow fever vaccine: stronger precautions in people with weakened immunity and those aged 60 years or older November 21, 2019 [Accessed 7 May 2025]
-
Lindsey NP, Rabe IB, Miller ER et al. Adverse event reports following yellow fever vaccination, 2007-13. J. Trav Med. Jul 4 2016;23 (5)
-
Kitchener S. Viscerotropic and neurotropic disease following vaccination with the 17D yellow fever vaccine, ARILVAX ((R)). Vaccine 2004; 22:2103-5.
-
McMahon AW. Eidex RB, Marfin AA et al. Neurologic disease associated with 17D-204 yellow fever vaccination: a report of 15 cases. Vaccine 2007;25: 1727-1734
-
Guimard T, Minjolle S, Polard E, et al. Short report: Incidence of yellow fever vaccine-associated neurotropic disease. Am J Trop Med Hyg 81:1141-3. 200913.
-
Centers for Disease Control and Prevention. Adverse events associated with 17D-derived yellow fever vaccination -United States, 2001-2002. MMWR 2002; 51: 989-993. [Accessed 7 May 2025]
-
Receveur MC, Bruyand M, Pistone T et al. Vaccination antiamarile: mise au point à propos des effets indésirables rares et graves [In French]. Médecine et Maladies Infectieuses 2009; 39(4):234-241.
-
MHRA: Yellow fever vaccine (Stamaril) and fatal adverse reactions: extreme caution needed in people who may be immunosuppressed and those 60 years and older [Accessed 7 May 2025]
-
Barwick Eidex R, for the Yellow Fever Vaccine Safety Working Group. History of thymoma and yellow fever vaccination. Lancet 2004; 11-17; 364 (9438): 936.
-
UK Health Security Agency, UK immunisation schedule: chapter 11. in Immunisation against infectious disease. 17 March 2022 [Accessed 7 May 2025]
-
Updated to include mention of MMRV vaccine, updated link to WHO documents.
-
Modelling data in risk areas updated and a new reference added.
-
Information for travellers leaflet added to resources.
-
Guidance on egg allergy and cardiac surgery involving incidental thymectomy added to vaccine information.
-
Reference links updated.
-
Risk for travellers updated to include information on a 2015 outbreak of yellow fever reported in Angola with imported cases reported from China, Democratic Republic of the Congo and Kenya.
Explore more
Malaria
Malaria is a serious and potentially life-threatening disease, transmitted to humans through the bite of infected female Anopheles spp. mosquitoes
Updated: 27 January 2026Sex and travel: sexually transmitted infections
Advice about reducing risk of sexually transmitted infections (STIs) during travel
Updated: 09 December 2025Pertussis (whooping cough) and travel
Information about pertussis and the UK vaccination regime
Updated: 10 July 2025Infectious diseases
Yellow fever
Yellow fever is caused by a virus, which circulates between infected monkeys or humans and mosquitoes
Updated: 18 February 2026Sex and travel: sexually transmitted infections
Advice about reducing risk of sexually transmitted infections (STIs) during travel
Updated: 09 December 2025Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes mosquito
Updated: 29 July 2025Preparing for healthy travel
Travel Insurance
Travellers must declare medical conditions when taking out travel insurance to ensure they are suitably covered
Updated: 06 December 2021Special risk travel/traveller
Travelling with additional needs and/or disability
This factsheet provides an overview and advice on the points to consider when travelling with additional needs and/or disability
Updated: 12 September 2025Areas of humanitarian crisis
For humanitarian aid workers and those advising those travelling to areas of conflict or disaster
Updated: 07 April 2025Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Updated: 11 March 2024Clinic resources
Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines
Information for health professionals on availability of vaccines and use of unlicensed products
Updated: 14 January 2026'Getting to Grips...' online events and video guides
Online guides and webinar sessions for health professionals interested in travel health
Updated: 16 December 2025The green book travel chapters
UK Health Security Agency Immunisation against infectious disease, the 'green book' travel chapter updates
Updated: 15 October 2024




