Insect and tick bite avoidance
Protection from insect and tick bites is essential to help prevent vector-borne diseases such as malaria, yellow fever and Zika

Key messages
-
Insect bites are relatively common in travellers, usually causing only minor irritation, but occasionally may cause more significant problems such as allergic reactions, secondary skin infections or transmission of infectious disease such as malaria, yellow fever, and Zika.
-
For many vector-borne diseases, avoiding insect bites is the only means of prevention. Where vaccines or malaria tablets are recommended, travellers should seek a pre-travel appointment with their health care provider.
-
Travellers should pack appropriate equipment for their destination; this may include protective clothing, insect repellents, mosquito nets, fine tipped tweezers and a first aid kit.
-
Insect repellent should be carried in hand luggage so it is available for use at transit stops, while disembarking, waiting for luggage and onward travel.
-
Many factors will affect the longevity of a repellent before reapplication is required. It is important to choose an effective active ingredient and reapply as soon as mosquitoes begin to take an interest (see below).
-
Travellers with a high fever of 38°C or more or other worrying symptoms should seek prompt medical advice. Malaria symptoms may occur up to a year after travel.
Overview
Insect and tick bites are relatively common in travellers, usually causing only minor irritation. However, bites can result in local skin damage, allergic reactions (ranging from small local reactions to life-threatening systemic reactions), secondary skin infections and spread of infectious diseases (vector-borne diseases) (see Table 1) [1-4].
Vector-borne diseases account for more than 17 percent of all infectious diseases. Every year diseases such as malaria, dengue, yellow fever and Japanese encephalitis cause more than 700,000 deaths globally [5]. The highest burden of disease occurs in tropical and subtropical areas where the poorest populations are disproportionately affected.
Vaccines or medications are available to help prevent a number of these diseases, but for many, bite avoidance is the only way to prevent infection.
Insect bites and stings
Arthropods include insects such as mosquitoes, gnats, flies and arachnids, such as spiders, mites and ticks [3]. The term 'insect' will be used here to include both insects and arachnids.
Insect bites or stings generally occur as a result of insect feeding (e.g. mosquitoes, bed bugs) or defence (e.g. bee and wasp stings or spider bites) and can range from being immediately painful to completely unfelt.
When an insect bites, substances such as anticoagulants (to prevent blood clotting) and vasodilators (to open blood vessels) are injected to ensure a flow of blood. These substances can lead to local skin or systemic reactions [3].
Bees, wasps and hornets are stinging insects and inject venom into the skin. Stings are usually painful immediately and the venom may cause reactions ranging from mild localised pain to severe systemic reactions including anaphylaxis (serious allergic reaction). In the UK, insect stings are the second most common cause of anaphylaxis outside of medical settings [3].
Insect vectors and diseases they transmit
Mosquitoes
The female mosquito requires a blood meal to reproduce. There are many species of mosquitoes, some bite during daylight hours (e.g. Aedes spp) and others are more active from dusk to dawn (e.g. Anopheles spp). The biting times of some mosquitoes can vary within the same species (e.g. Anopheles mosquitoes which transmit malaria) [6].
Mosquitoes are attracted by several factors, including the presence of carbon dioxide (from skin and breath), heat (from skin), odours (including fragrances from perfumes and soaps), lactic acid and movement; some individuals may also be more attractive to mosquitoes than others [7].
Ticks
Ticks typically live on the ground in long grassy areas and usually feed on small mammals. They become attached to humans after brushing against grass, after which they crawl on skin or clothing until they find a suitable place to attach and feed, often at a skin fold in the groin, under the arm, at the scalp line or at the edge of underclothes. The bite is generally painless [8]. As prompt removal of ticks may prevent transmission of some infectious diseases, it is important to check for ticks on the body after outdoor activities.
Table 1. Examples of diseases transmitted to humans by mosquitoes, ticks and other vectors [5]
| Vector | Vector-borne diseases | |
| Mosquitoes | Anopheles spp | Malaria Lymphatic filariasis |
| Aedes spp | Chikungunya Dengue fever Eastern equine encephalitis La Cross encephalitis Lymphatic filariasis Rift Valley fever Ross River virus Yellow fever Zika |
|
| Culex spp | Japanese encephalitis Lymphatic filariasis Ross River virus St Louis encephalitis West Nile virus |
|
| Ticks | Babesiosis Borreliosis Crimean Congo haemorrhagic fever Lyme disease Rickettsial diseases (spotted fever, Q fever) Rocky mountain spotted fever Tick-borne encephalitis Tularemia |
|
| Flies | Tsetse Fly | African trypanosomiasis |
| Sand Fly | Leishmaniasis | |
| Black Fly | Onchocerciasis | |
| Fleas | Plague Murine typhus |
|
| Reduviid bug | American trypanosomiasis (Chagas disease) | |
| Lice | Louse-borne relapsing fever Typhus |
|
| Chigger Mites (Trombiculid mites) |
Scrub typhus | |
Bed bugs
There has been a resurgence of bed bug infestations in recent years [9]; there is no evidence that they transmit disease-causing pathogens. There are few published studies investigating the role of insect repellents in protecting against bed bug bites [10].
Travellers should be encouraged to inspect their sleeping accommodation for bed bugs on mattresses and bedding, which might present as blood spotting on linens; keep suitcases or rucksacks off the floor when not in use and inspect clothing before replacing them in luggage [10].
Risk for travellers
The risk of insect bites, and possible vector-borne disease, to the traveller will depend on exposure to insects. This will be determined by destination, season and rainfall patterns, as well as activities undertaken, length of stay and measures taken to avoid insect bites. Destination-specific information on some of the diseases spread by insects can be found on the Country Information pages.
Vaccines and tablets are available to help protect against some of the diseases, but may not be suitable for all travellers, placing them at higher risk of disease. Avoiding bites from insects and ticks may be the only way to reduce the risk of disease.
Before travel
Travellers should research their destination to determine possible risks for vector-borne diseases (see our Country Information pages). Vaccinations and/or malaria tablets may be recommended, in which case a pre-travel appointment should be booked with a health care provider ideally four to six weeks before departure. Although last-minute advice is still useful if time is short.
Travellers should consider if they need to pack protective clothing, insect repellents, insecticide treated bed/cot nets, plug-in insecticides and a first aid kit with items to manage insect bites, for example fine-tipped tweezers to remove ticks, painkillers and antihistamine tablets and/or cream to reduce itching.
During travel
Travellers should be advised to protect themselves against insect and tick bites day and night depending on the vector and risk of disease at destination. Indoor and outdoor biting can occur, including inside cars and other vehicles and at airports [6]. A combination of the measures recommended below are the most effective way to prevent bites.
Key points to reduce insect and tick bites:
- Avoid areas of stagnant or standing water, where mosquitoes are likely to breed.
- Keep to footpaths and avoid long grass when walking to avoid tick bites.
- Check body for ticks after outdoor activity and remove them promptly (see below).
- Wear loose-fitting clothing, with long sleeves, long trousers, tucked into socks.
- Light coloured clothing will help see ticks and other insects, avoid dark blue clothing where tsetse fly is present [11]. There is no evidence that the colour of clothing is relevant to mosquitoes [6].
- Clothing can be sprayed or impregnated with insecticide (e.g. permethrin) or purchased pre-treated to reduce biting through clothing. These treatments can provide a high level of bite prevention. Alternatively DEET based repellents can be applied to natural fibres such as cotton, but may damage synthetic fabrics including items like plastic watch jewellery [6].
- Use insect repellents on exposed skin (even if clothing has been treated): DEET based repellents are considered the most effective currently available. If DEET is not tolerated (or is not available), an alternative preparation should be used (see below).
- In areas with vector-borne diseases, use air conditioning where available or sleep in screened accommodation, under a mosquito net impregnated with insecticide.
- Insecticide vaporisers can be used to inhibit mosquito bites and mosquito coils can be used outdoors (they are not recommended indoors).
- For those staying long-term in areas with vector-borne diseases it is possible to reduce mosquito breeding sites around the home by removing any pools of water in ditches, plant pots, gutters, drains and rubbish collected in the area.
Insect repellents
Many factors affect how long insect repellent is effective. These include the number of mosquitoes or insects present, sweat causing run off of repellent, swimming, type of mosquito/insect and any mosquito or insect 'attractants' produced by the individual traveller. Insect repellent sweat-off time varies with activity (e.g. inactivity versus vigorous exercise) [6] and humidity at the destination.
DEET
DEET (N, N-diethyl-m-toluamide) has been used as an insect repellent for more than 50 years. A number of studies have concluded that the risks of adverse effects from DEET are low for all groups, including infants and children as well as pregnant and breastfeeding women, when applied according to the product instructions [6, 12].
Repellent containing DEET, at 50 percent concentration, is recommended for all travellers over two months provided it can be tolerated. There is no further increase in duration of protection beyond a concentration of 50 percent [6].
The interval between re-application of repellent will depend on the DEET formulation and concentration used. In practice, travellers apply around half of the amount at which a product has been tested, therefore more frequent application will be required. Repellents may also need to be reapplied more regularly, for example after swimming and in hot, humid conditions when they may be removed by perspiration. As a guide, travellers should reapply repellents when the mosquitoes begin to 'take an interest', to ensure that they do not bite. Some products can be sprayed onto clothing; DEET may melt synthetic fibres [6].
DEET and sunscreen
Several studies have shown that DEET decreases the protection of SPF 15 sunscreen, although there is no evidence that sunscreen reduces the efficacy of DEET when used at concentrations above 33 percent [6]. When both are required, DEET should be applied after the sunscreen, and 30 to 50 SPF sunscreen should be used to compensate for the reduction in SPF induced by DEET [6, 13].
Alternatives to DEET
If DEET is not tolerated (or unavailable), and travellers are visiting areas where malaria or other vector-borne diseases are present, a repellent containing one of the following three active ingredients repellents should be used as an alternative, at the highest strength available.
Icaridin (Picaridin)
Icaridin has repellent properties similar to DEET with a comparable duration of protection when both are used at 20 percent. If used for mosquito bite prevention against malaria, at least a 20 percent preparation is advised [6].
Eucalyptus citriodora oil, hydrated, cyclized.
This active ingredient provides effective protection for several hours and was previously known as p-menthane 3,8 diol or PMD. However, the duration of protection is shorter than DEET so more frequent application is required. Care should be taken when applying as accidental application to the eyes can result in damage [6].
3-ethlyaminopropionate (IR3535)
3-ethlyaminopropionate (IR3535) has a shorter duration of protection against Anopheles mosquitoes than DEET, and so more frequent application is required, but it is still an effective repellent. Care should be taken when applying as accidental application to the eyes can result in damage [6].
Use of insect repellents in pregnancy and breastfeeding
Avoidance of mosquito bites is extremely important in pregnancy as pregnant women are particularly attractive to mosquitoes [6].
The use of 20 percent DEET during the second and third trimesters of pregnancy was not associated with adverse effects on the infants in pregnancies followed for up to 12 months after birth [6, 13]. Because malaria is a serious disease in pregnancy, DEET based repellents in concentrations up to 50 percent are recommended for all pregnant women, at any stage of pregnancy, travelling to areas where malaria or other insect-borne diseases are a risk [6, 14].
Icaridin and eucalyptus citriodora oil are alternatives to DEET. However, there is no data concerning exposure in human pregnancy, although animal studies have not demonstrated any features of maternal or developmental toxicity [14].
DEET may also be used in concentrations up to 50 percent in breastfeeding. Nursing mothers should wash repellents off their hands and breast skin before handling infants.
Use of insect repellents in infants
Recommendations on the use of DEET in young children vary between countries. According to UK Health Security Advisory Committee on Malaria Prevention (ACMP) DEET may be used at a concentration of up to 50 percent in babies and children aged over two months. If a particular DEET manufacturer's product information recommends a higher age cut off for use in children, the ACMP guidance should be followed. DEET is not recommended for babies under two months of age. Instructions on application should be followed. Babies under two months should be protected with protective clothing and insecticide treated nets draped over cots and prams, secured around the edges to avoid gaps [6].
Children should not be allowed to handle repellents as they may inadvertently ingest them or get them in their eyes. Adults should apply repellent to their own hands, then onto the child's skin, and avoid applying to children's hands [6].
How to use insect repellents safely [6]:
- Do not use over cuts, irritated or inflamed skin.
- Do not apply directly to the face - apply repellent to hands, then to the face to avoid contact with lips and eyes. Wash hands after application.
- Do not apply to children's hands.
- Apply and re-apply repellents when mosquitoes begin to land, bearing in mind the manufacturers' instructions.
- Remove with soap and water when repellent is no longer needed.
- Ensure repellents are not ingested or inhaled.
- DEET can be used in concentrations of up to 50 percent in pregnant and breastfeeding women, and in infants and children older than two months (unless allergic).
- When sunscreen and DEET are needed, DEET should be applied after sunscreen (use 30 - 50 SPF sunscreen to compensate for reduction in SPF induced by DEET).
- DEET may damage plastics and artificial fibres so care is needed to avoid contact. DEET does not damage natural fibres such as wool, linen or cotton.
- Picaridin, eucalyptus citriodora oil (PMD) or 3-ethlyaminopropionate (IR3535) based repellents are available for those who prefer not to use DEET-based products. Picardin should be used in concentrations of at least 20 percent.
Mosquito nets
All travellers to malaria-endemic areas should sleep under a mosquito net to avoid being bitten, unless the room is well screened or with working, switched on air-conditioning where mosquitoes cannot enter. If the room door has been opened, the room should then be checked for mosquitoes. Most nets now available are long-lasting insecticide impregnated nets, which have an expected useful life of at least three years [6]. Nets other than long-lasting nets will need to be impregnated with insecticide (e.g. permethrin) every six to twelve months to remain effective, depending on the frequency of washing. The product instructions should always be followed [6].
Mesh size in mosquito bed nets should be no larger than 1.5mm and nets should be kept in good condition, free from tears and tucked in under the mattress, so they are taut. It may be useful for travellers to carry a small sewing kit so that repairs can be made if the net develops a hole. Extra equipment for hanging the net can be helpful including extra string or wire hooks.
Room protection (including air conditioning and screening)
Doors and windows to sleeping accommodation should be screened with fine mesh.
Air conditioning reduces night-time temperature and increases air flow in a building and therefore can reduce likelihood of insect and mosquito bites. Ceiling fans reduce the nuisance from mosquitoes [6].
An insecticide called Permethrin (and other similar products called synthetic pyrethroids) have a rapid knock-down effect on mosquitoes and can be used to kill resting mosquitoes in a room. Permethrin can also be used to treat clothing [6] but this insecticide should not be used directly on skin.
There is evidence that insecticide vaporisers inhibit mosquito bites and cause mosquito repellence and knockdown [12]. During the night, if electricity is available, a plug-in proprietary heated liquid reservoir device containing insecticide or a plug-in electrically heated device to vapourise a 'mat' (tablet) containing a synthetic pyrethroid can be used [6].
A systemic review demonstrated that mosquito coils can decrease bites by repelling and killing mosquitoes [15]. Burning a coil containing a synthetic insecticide may be useful for some travellers but they must only be used outdoors [6].
Room protection is important in malaria prevention but should not be used in isolation.
Measures not recommended for repelling insects [6]
There is no evidence that any of the following products, have repellent effect on mosquitoes [6]:
- Garlic.
- Vitamin B1.
- Vitamin B12.
- Brewer's yeast tablets and other vitamins.
- Yeast extract (e.g. Marmite).
- Electronic buzzers.
- Mobile phone apps.
- Tea tree oil or proprietary bath oils/emollients.
- Alcohol/tonic water (the amount of quinine in tonic water has no effect on malaria parasites).
- Homeopathy/herbal remedies.
- Citronella oil-based repellents due to their short duration of action; they have been withdrawn in Europe.
- Heavy metal music [6].
Management of insect and tick bites
In addition to spreading infectious diseases, complications from insect bites and stings include local skin damage, allergic reactions and secondary bacterial infection.
Reactions from most insect bites or stings will improve within hours or days. Clean the bite site with soap and water. Using a cold compress (if available) may provide relief from pain or itching [3, 16]. The cold pack should have a cloth barrier between the ice and skin to prevent damaging skin tissue. Applying the ice pack on and off at 15 minute intervals is a common regimen [4].
Try not to scratch insect or mosquito bites and keep them clean and dry to avoid infection. Antiseptic and basic wound dressings can be helpful if the bite is causing irritation and likely to become infected.
Following an insect sting, if the stinger is still visible in the skin, remove it as quickly as possible by scraping sideways with a fingernail or piece of card.
Pain relief tablets (e.g. paracetamol and ibuprofen) are often recommended to ease pain, although there is a lack of evidence to support these treatments [3]. Itching may be reduced by taking antihistamine tablets or applying a mild steroid cream directly to the skin, although good quality evidence to support their use is lacking [3].
Ticks need to be removed from the skin very carefully. This can be done with fine tipped tweezers or specially designed tick removers (see Figure 1).
The tick should be grasped as close to the skin surface as possible and pulled steadily upwards, taking care not to crush the tick's body or squeeze the stomach contents into the site of the bite. After removing the tick, the bite area should be cleaned thoroughly with soap and water, or iodine/antiseptic if available. If tick mouthparts are not fully removed, persistent nodules (small lumps) can develop [3].
The tick should not be covered with solutions such as nail varnish or petroleum jelly and heat should not be used for tick removal.
Figure 1. How to remove a tick
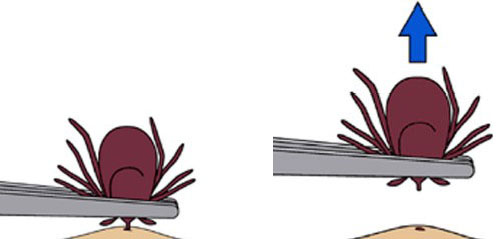
Source: CDC. Tick removal
After travel
Those with a fever (38°C or more) or other worrying symptoms after travel should seek urgent medical help, remembering to tell their doctor or other health professional about all the countries they travelled to. Malaria symptoms can appear up to a year after travel.
If a rash or fever develops within several weeks of removing a tick, medical attention should be sought, providing details of the recent tick bite, including when and where the bite occurred.
Insect bites can sometimes get infected, becoming swollen, painful and red with pus where the bite occurred. Travellers should contact their GP or pharmacist if they are concerned about the symptoms; antibiotics may be required.
Resources
- UK Health Security Agency, Advisory Committee on Malaria Prevention: Guidelines for malaria prevention in travellers from the United Kingdom
- Goodyer L, Croft A, Frances S, et al. Expert review of the evidence base for arthropod bite avoidance. J Trav Med. 2010; 17:182-92
- Lupi E, Hatz C, Schlagenhauf P., The efficacy of repellents against Aedes, Anopheles, Culex and Ixodes spp. - a literature review. Travel Med. Infect. Dis. Nov-Dec 2013; 11(6):374-411
- NHS: Insect bites and stings
- UK Health Security Agency: Mosquito bite avoidance for travellers
- UK Health Security Agency: Ticks bite risks and prevention of Lyme disease: resources
- TravelHealthPro: Malaria resources
- WHO: Vector-borne diseases
References
-
Schlagenhauf P, Weld L, Goorhuis A et al. Travel-associated infection presenting in Europe (2008-12): an analysis of EuroTravNet longitudinal, surveillance data, and evaluation of the effect of the pre-travel consultation. Lancet Infect Dis. 2014; 15(1): 55-64.
-
Hochedez P, Caumes E. Common Skin Infections in Travelers. J. Travel Med. 2008; 15(4): 252-62
-
National Institute for Health and Care Excellence, Clinical Knowledge Summaries. Insect bites and stings. Last revised July 2023 [Accessed 21 March 2024]
-
BMJ Best Practice. Insect bites and stings. British Medical Journal. Last reviewed 14 February 2024 [Accessed 21 March 2024]
-
World Health Organization. Vector-borne diseases Factsheet. Last updated March 2 2020 [Accessed 21 March 2024]
-
UK Health Security Agency, Advisory Committee on Malaria Prevention (ACMP), Guidelines for malaria prevention in travellers from the United Kingdom Last updated 16 January 2024. [Accessed 21 March 2024]
-
Fradin MS. Insect Protection in Keystone JS (ed). Travel Medicine. 3rd ed. Elsevier: 2013.
-
European Centre for Disease Prevention and Control. Personal protective measures against tick bites. January 2015 [Accessed 21 March 2024]
-
Mutebi J and Gimnig J. Mosquitoes, Ticks and Other Arthropods. Chapter 3 in Centers for Disease Control and Prevention. Health Information for International Travel 2024. Last reviewed 1 May 2023. Oxford University Press [Accessed 21 March 2024]
-
Webb CE. Can travellers avoid bed bug bites? Travel Med Infect Di. 2012; 10(5-6): 281-2.
-
Burri C, Chappuis F and Brun R. Human African Trypanosomiasis in Farrar J (ed). Manson's Tropical Diseases. 23rd ed. Elsevier, 2014.
-
Goodyer L, Croft A, Frances S et al. Expert review of the evidence base for arthropod bite avoidance. J Trav Med. 2010; 17(3):182-92.
-
Murphy M, Montemarano AD, Debboun M et al. The effect of sunscreen on the efficacy of insect repellent: a clinical trial. J Am Acad Dermatol. 2000; 43(2 Pt 1): 219-22.
-
UK Teratology Information Service. Chemical Insect Repellents. May 2018 [Accessed 21 March 2024]
-
Lawrence C, Croft A. Do mosquito coils prevent malaria? A systemic review of trials. J Travel Med. 2004 11(2): 92-6.
-
Management of simple insect bites: where's the evidence? Drugs and Therapeutics Bulletin 2012; 50(4): 45-8. [Accessed 21 March 2024]
Explore more
First aid kits
A travel health first aid kit is recommended for travellers
Updated: 03 September 2024Infectious diseases
Yellow fever
Yellow fever is caused by a virus, which circulates between infected monkeys or humans and mosquitoes
Updated: 18 February 2026Sex and travel: sexually transmitted infections
Advice about reducing risk of sexually transmitted infections (STIs) during travel
Updated: 09 December 2025Chikungunya
This viral infection occurs in some tropical and subtropical regions of the world, predominantly transmitted through the bite of an infected Aedes mosquito
Updated: 29 July 2025Preparing for healthy travel
Travel Insurance
Travellers must declare medical conditions when taking out travel insurance to ensure they are suitably covered
Updated: 06 December 2021Special risk travel/traveller
Travelling with additional needs and/or disability
This factsheet provides an overview and advice on the points to consider when travelling with additional needs and/or disability
Updated: 12 September 2025Areas of humanitarian crisis
For humanitarian aid workers and those advising those travelling to areas of conflict or disaster
Updated: 07 April 2025Sickle cell disease and thalassaemia
Information on pre-travel preparation, tips to stay health abroad and links to useful resources for travellers with sickle cell disease and thalassaemia
Updated: 11 March 2024Clinic resources
Vaccines and medicines: availability, supply, shortages and use of unlicensed medicines
Information for health professionals on availability of vaccines and use of unlicensed products
Updated: 14 January 2026'Getting to Grips...' online events and video guides
Online guides and webinar sessions for health professionals interested in travel health
Updated: 16 December 2025The green book travel chapters
UK Health Security Agency Immunisation against infectious disease, the 'green book' travel chapter updates
Updated: 15 October 2024




